Introduction
Oral cancer represents a significant global health burden, ranking as the sixth most prevalent cancer worldwide. Over 640,000 new cases are diagnosed annually, and survival rates heavily depend on the stage of detection. Early-stage diagnosis can elevate survival rates from a dismal 32% to over 80%. However, late detection remains the norm due to reliance on subjective diagnostic methods, delayed access to care, and a lack of standardized tools. The advent of artificial intelligence (AI) promises to address these challenges, transforming oral cancer diagnostics with unparalleled accuracy, efficiency, and accessibility.
Traditional Oral Cancer Detection Methods: Strengths and Limitations
Oral cancer detection has historically relied on a mix of clinical and laboratory techniques, each with unique benefits and shortcomings:
- Visual Examination:
- Strengths: Easy to perform during routine dental check-ups.
- Limitations: Highly subjective and prone to inaccuracies, especially in detecting early or subtle lesions.
- Biopsy:
- Strengths: The gold standard for diagnosis, offering histopathological confirmation.
- Limitations: Invasive, time-consuming, and reliant on specialized expertise.
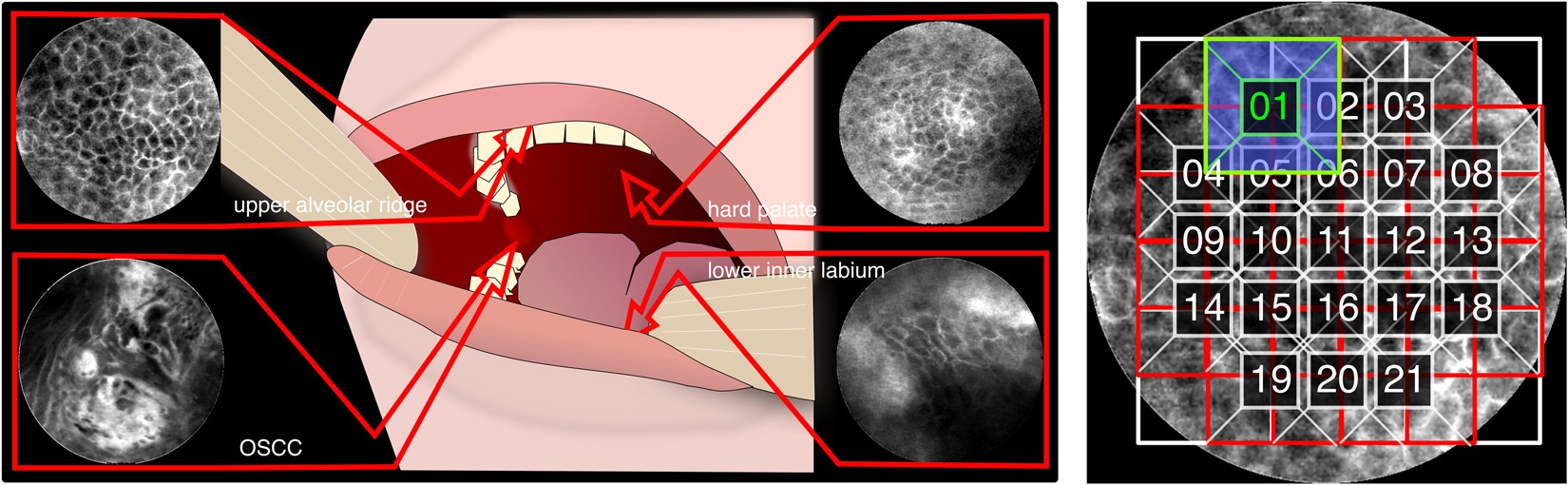
- Imaging Techniques: Autofluorescence and optical coherence tomography (OCT) are used to identify abnormal tissue. However, they suffer from low specificity and limited adoption due to cost and accessibility issues.
- Emerging Methods: Salivary biomarkers and laser diagnostics show potential but remain costly and require further validation for widespread use.
These traditional methods, while critical, often fail to provide rapid, cost-effective, and accurate results in real-world settings.


The AI Revolution in Oral Cancer Detection
AI technologies, particularly machine learning (ML) and deep learning (DL), are transforming oral cancer diagnostics by addressing the limitations of traditional approaches. Key contributions of AI include:
- Enhanced Accuracy:
- AI models such as Convolutional Neural Networks (CNNs) excel in analyzing complex datasets, particularly medical images.
- Detection accuracies for oral lesions range from 80% to 100%, often surpassing human performance. Models like DenseNet121 and EfficientNet-B0 achieve high specificity and sensitivity, effectively distinguishing malignant from benign tissues.
- Cost-Effectiveness:
- Smartphone-based AI tools allow for point-of-care diagnostics, especially in low-resource settings. Images captured on standard devices can be analyzed using deep learning algorithms, reducing dependence on expensive equipment or procedures.
- Smartphone-based AI tools allow for point-of-care diagnostics, especially in low-resource settings. Images captured on standard devices can be analyzed using deep learning algorithms, reducing dependence on expensive equipment or procedures.
- Improved Patient Outcomes:
- By providing rapid, accurate diagnoses, AI facilitates early intervention, improving survival rates and reducing treatment complexity.
- AI enables personalized care through predictive analytics, helping clinicians anticipate treatment outcomes and plan more effectively.
Real-World Applications of AI in Oral Cancer Detection
AI’s practical impact on oral cancer detection is already evident in several domains:
- Smartphone-Based Screening: AI-powered tools analyze images captured via mobile phones, making screening accessible in remote or underserved regions. A clinical study demonstrated an 80.6% agreement between smartphone-based AI diagnoses and standard methods.
- Telemedicine: AI bridges the gap between patients in rural areas and specialized care. Local healthcare providers capture and upload diagnostic images for remote analysis by experts, democratizing access to quality healthcare.
- Workflow Optimization: AI systems automate image enhancement, segmentation, and lesion classification, reducing diagnostic delays and easing the burden on healthcare professionals.
Challenges in AI Implementation
Despite its potential, AI in oral cancer detection faces several challenges:
- Data Limitations: AI models require large, diverse, and annotated datasets to achieve reliable performance. Limited availability of such data hampers model training and generalizability.
- Ethical and Privacy Concerns: Ensuring patient data privacy and algorithm transparency is critical. Establishing robust regulatory frameworks will be essential for ethical AI adoption.
- Integration into Clinical Practice: Seamless integration of AI tools into existing workflows demands collaboration between developers, clinicians, and policymakers. Training healthcare professionals to utilize AI effectively is also vital.
The Road Ahead: Addressing Challenges and Unlocking AI’s Full Potential
To fully realize AI’s transformative potential in oral cancer care, several steps must be prioritized:
- Data Standardization and Sharing: Developing large, open-access databases of annotated images can improve AI model training and validation, ensuring robustness across diverse populations.
- Regulatory Frameworks: Establishing clear guidelines around data privacy, algorithm accountability, and clinical validation is critical for safe and ethical AI deployment.
- Global Collaboration: Partnerships between governments, research institutions, and private sectors can drive innovation, funding, and widespread implementation of AI solutions.
Conclusion
AI is revolutionizing the detection and management of oral cancer, offering tools that enhance diagnostic accuracy, speed, and accessibility. While not a replacement for healthcare professionals, AI serves as a powerful ally, augmenting clinical decision-making and improving patient outcomes. Addressing challenges like data limitations, ethical concerns, and workflow integration will be key to unlocking AI’s full potential. With continued innovation and collaboration, AI promises to make early oral cancer detection a global standard, reducing the disease’s burden and saving countless lives.
The future of oral cancer care is here, and it’s powered by AI.